IBM’s new Imaging AI Orchestrator offers a cloud-native AI subscription service for scalable, regulatory-approved AI imaging applications.
We are entering an exciting era of medicine, where big data and artificial intelligence/machine learning (AI/ML) can help clinicians find better ways to treat patients. Yet, despite the promise of AI to revolutionize health care, systems have hit many roadblocks on the path to implementing advanced data analytics into the diagnosis and treatment of disease.
As new tools emerge, clinicians and health care institutions are left with many unanswered questions. How can clinicians implement distinct tools from multiple vendors into hospital and institution workflows? Will tools be user friendly enough for clinicians with limited IT and AI knowledge to navigate them? And how will AI tools realistically support existing clinical decisions?
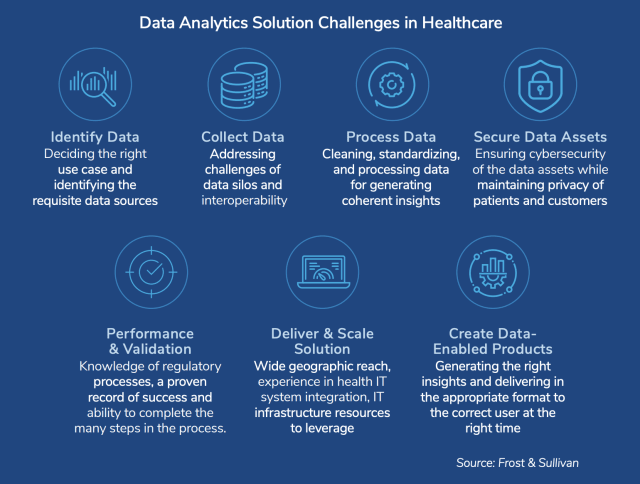
Frost & Sullivan, in partnership with IBM, recently published an infographic on imaging AI, which highlights some of the many challenges currently faced by health care institutions looking to adopt advanced imaging applications. For example, before an institution can implement an AI tool, it needs to provide a clinical benefit and advanced security to protect patient data. So, for a tool to supplement clinical decisions, it must be accurate, functional and secure.
With physicians busy visiting patients and making clinical decisions, how can institutions find the time and expertise to individually evaluate the many emerging AI tools? Recently, IBM Watson Health launched a clever solution to this problem: the IBM Imaging AI Orchestrator. The software is a cloud-based AI service that provides health care systems with access to scalable, regulatory-cleared AI applications. IBM manages multiple applications within the system to deliver easily accessible, secure AI solutions for imaging operations.
Why Do Healthcare Systems Need AI?
Health care is a data-driven industry, and all clinics currently possess rich datasets of patient information, with details on population factors, disease outcomes, clinical trial data, imaging diagnostics and more. If clinics could intelligently use this wealth of data, it could improve productivity and accuracy.
This is where AI and ML come in, poised to help clinics identify patterns in existing data and support clinical decision-making. Advanced data analytics can often identify patterns and insights that are not obvious to the human eye.
Interestingly, AI can not only support clinical outcomes but can also identify bottlenecks within the health care system to help improve efficiency and the overall patient experience. This can allow physicians to focus on their clinical work, while AI can highlight areas of a given workflow that can be modified to improve patient care.
Plus, health care data often exists in distinct formats and systems, making it difficult to identify patterns within a patient’s personal health history. AI and ML can help connect these diverse datasets to further support clinical outcomes and provide clinicians with a clearer picture of a patient’s health.
IBM Watson Health Takes the Guess Work Out of AI Application Adoption
When it comes to AI tools for health care, new applications are constantly emerging to tackle distinct problems. Currently, more than 90 companies have received regulatory approval for clinical AI applications. There are more than 250 vendors in radiology alone, and most are start-ups. The rapidly evolving landscape creates a unique challenge for clinicians looking to gain AI-based insights as part of their imaging analysis workflow.
Currently, clinicians need to individually consider tools for their clinical relevance, their ability to be integrated into existing imaging systems, and whether a tool can be supported by existing IT and picture archiving and communications systems (PACS). Physicians are already tasked with long patient lists and life-saving decision-making. It can be burdensome to ask a health care team to rigorously evaluate the rapidly evolving world of AI imaging tools.
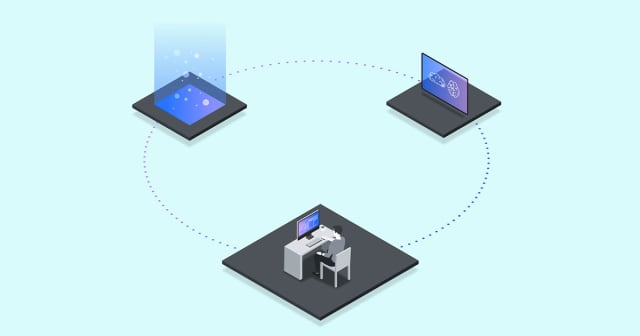
To help facilitate the adoption of AI in health care settings, the IBM Imaging AI Orchestrator is a user-friendly AI service that provides access to a suite of proven AI applications for clinical imaging services. The AI tools within the Imaging AI Orchestrator are specified for various applications and are curated by IBM to meet strict privacy, security and regulatory requirements.
The system integrates seamlessly with existing workflows and delivers aggregated results reports directly to PACS. Therefore, within a physician’s existing reading process, the AI service makes it easy to access AI insights.
“We recognize that when it comes to applying AI in imaging, it’s hard to go it alone,” said David Gruen, MD, MBA, FACR, chief medical officer of Imaging at Watson Health. “Because each AI application is developed in a unique way with a specific purpose, it can be challenging for organizations to review and assess each one, and then to deploy them in a way that’s beneficial to radiologists and their patients. That’s why, with the rapid proliferation of approved algorithms, staffing shortages, and complexity of disease, the IBM Imaging AI Orchestrator could not come at a better time.”
An Orchestrator to Simplify Health Care IT
Beyond the clinic, a major goal of the Imaging AI Orchestrator is to deliver a service that could realistically help health care organizations integrate multiple new tools into their existing workflows.
Previously, when an organization or institution wanted to introduce a new AI tool, the IT department would need to establish a protocol, integrate the tool into their workflow and manage any upgrades or maintenance. The Orchestrator now makes it easy to integrate new applications into existing PACS systems.
The vendor-neutral AI service standardizes the deployment of AI applications to help tools scale within a health care system. The entire service is built on IBM’s hybrid cloud infrastructure and complies with health care data standards, including DICOM and HL7. The system is cloud native and uses intelligent edge devices, requiring minimal changes to the current IT infrastructure of health care institutions.
When it comes to updating tools, the service monitors the industry to include new tools as they are rigorously tested and approved for clinical use. The IBM Imaging AI Marketplace includes all the applications available through the service that are regulatory approved and security vetted.
The service already includes many tools for clinical applications. For example, behold.ai and its red dot algorithm are available through the AI Orchestrator. The AI application can rapidly identify abnormalities in chest x-rays and triage for pneumothorax on X-ray images with high accuracy. In addition, cortechs.ai offers NeuroQuant to process volumetric MRI images. By comparing such images to reference images, the software can assist with the detection of Alzheimer’s, Multiple Sclerosis, dementia and more. Other tools are available for applications in cardiology, radiology and beyond.
IBM Imaging Workflow Orchestrator
Another recent announcement from IBM is its new Imaging Workflow Orchestrator, software that helps streamline clinicians’ readings by integrating clinical trials, patient data and AI outputs into one user-friendly interface. The cloud-native software as a service (SaaS) improves physicians’ access to the academic literature and imaging data.
The experience can be customized to individual radiologists and is compatible with local, remote, telehealth and distributed clinical settings. The interface can include as many AI inputs as clinicians determine to support decision-making and improve physician confidence and efficiency.
“These innovative offerings are designed to provide health systems and radiology practices with a smarter way to adopt AI for diagnostic imaging and to improve the reading experience. For health systems, they can help to deliver quality patient care. By supporting physicians and specialists to be more productive by using AI augmented tools, patients have more confidence. For radiology practices, orchestrating AI and workflows can expand their capacity to provide imaging services at a pace to meet today’s growing healthcare demands,” said Alok Gupta, vice president and general manager of IBM Watson Health Imaging.
AI Applications Are Poised to Transform Modern Medicine But Concerns Remain
In recent years, AI has emerged as a powerful approach to data analytics, promising to radically change almost every industry. Health care is no exception, and many clinicians are excited by the prospect of powerful AI applications supporting clinical decision-making. Not only can AI applications identify overarching patterns in data, but they also stand to increase health care efficiency and productivity when integrated into triage and workflow pipelines.
However, the use of AI in health care also presents several challenges. Beyond the obvious concerns about security and accuracy, AI and ML trained on clinical datasets will often integrate explicit and implicit bias within their algorithms.
In addition, data analytics can often inadvertently integrate systemic racism into outputs, resulting in poorer patient health outcomes. The National Institute for Health Care Management (NIHCM) Foundation published a helpful summary graphic describing the major concerns with racial bias in intelligent health care tools.
As AI applications look to continuously improve, a crucial development area will be critically assessing input data and ensuring that outputs do not introduce further bias into the health care system.